2014 Lesotho DHS Shows Great Improvements, but Focus on HIV Remains
 Many DHS surveys include HIV testing. In some countries, the resulting HIV prevalence data prove to be a distraction; there is more attention on an unchanged 1% HIV prevalence rate than on the tremendous malaria burden or a high child mortality rate. The 2014 Lesotho DHS (LDHS), however, is a very different case. While the 2014 LDHS highlights the country’s great progress in health facility births, family planning use, and child survival, HIV prevalence among adults age 15-49 is a staggering 25%. Not surprisingly, this was the only topic that received any press coverage following the June 15, 2016, LDHS national seminar.
Many DHS surveys include HIV testing. In some countries, the resulting HIV prevalence data prove to be a distraction; there is more attention on an unchanged 1% HIV prevalence rate than on the tremendous malaria burden or a high child mortality rate. The 2014 Lesotho DHS (LDHS), however, is a very different case. While the 2014 LDHS highlights the country’s great progress in health facility births, family planning use, and child survival, HIV prevalence among adults age 15-49 is a staggering 25%. Not surprisingly, this was the only topic that received any press coverage following the June 15, 2016, LDHS national seminar.
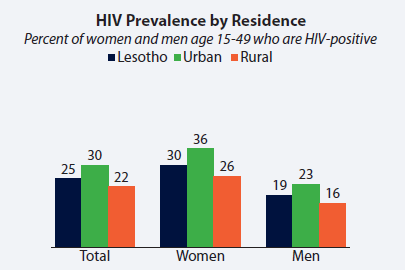 Many Basotho, including those representing the Ministry of Health and agencies that provide HIV-related funding and program assistance, had been hoping to see a decline in HIV prevalence relative to 2009, the last time for which a national HIV prevalence estimate had been released. However, the 2014 data indicate that nationally, the prevalence has remained stable, while among women it has increased from 27% in 2009 to 30% in 2014.
Many Basotho, including those representing the Ministry of Health and agencies that provide HIV-related funding and program assistance, had been hoping to see a decline in HIV prevalence relative to 2009, the last time for which a national HIV prevalence estimate had been released. However, the 2014 data indicate that nationally, the prevalence has remained stable, while among women it has increased from 27% in 2009 to 30% in 2014.
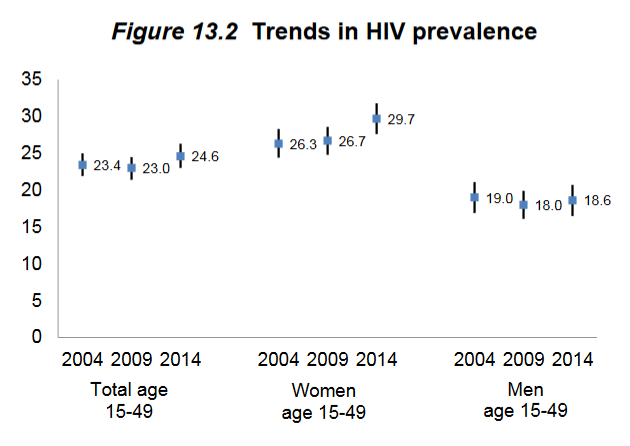 Some stakeholders saw optimism in these figures: a higher HIV prevalence may be the result of more HIV-positive women receiving anti-retroviral (ARV) therapy, and thereby surviving much longer than they would have without ARVs. But of course, higher prevalence can also be due to more new infections. The LDHS also tested blood samples for HIV incidence, and these data were published as part of the Final Report for the first time ever in a DHS survey. The 2014 LDHS reports an HIV incidence rate of 1.9 new infections for every 100 person-years of exposure. In other words, for every 100 people, there is an average of 1.9 new infections per year. Despite prevention efforts, new infections are indeed entering the population.
Some stakeholders saw optimism in these figures: a higher HIV prevalence may be the result of more HIV-positive women receiving anti-retroviral (ARV) therapy, and thereby surviving much longer than they would have without ARVs. But of course, higher prevalence can also be due to more new infections. The LDHS also tested blood samples for HIV incidence, and these data were published as part of the Final Report for the first time ever in a DHS survey. The 2014 LDHS reports an HIV incidence rate of 1.9 new infections for every 100 person-years of exposure. In other words, for every 100 people, there is an average of 1.9 new infections per year. Despite prevention efforts, new infections are indeed entering the population.
There is still good news in the HIV community in Lesotho. Voluntary testing programs are far-reaching: more than 80% of women and 60% of men in Lesotho have ever tested for HIV and received the results, up from 66% of women and 37% of men in 2009. Eighty percent of women who gave birth in the two years before the survey received HIV counseling during antenatal care, and 79% also were tested for HIV and received the results.
The positive effects of voluntary medical male circumcision are also demonstrated by the 2014 LDHS data: only 14% of men who were medically circumcised tested positive for HIV compared to 21% among those were not circumcised or were traditionally circumcised only.
 The 2014 LDHS has 17 chapters. Only 2 of them are about HIV. And yet, it’s very hard to get attention on child mortality, nutrition, gender issues, or family planning when 25% of the adult population has HIV. And HIV does not exist in a vacuum; it affects the health of this country in many indirect ways as well. Child mortality is affected by children’s HIV status, as well as the status of their parents; HIV prevention behaviors must be considered within the lens of gender issues; and family planning cannot be separated from HIV education.
The 2014 LDHS has 17 chapters. Only 2 of them are about HIV. And yet, it’s very hard to get attention on child mortality, nutrition, gender issues, or family planning when 25% of the adult population has HIV. And HIV does not exist in a vacuum; it affects the health of this country in many indirect ways as well. Child mortality is affected by children’s HIV status, as well as the status of their parents; HIV prevention behaviors must be considered within the lens of gender issues; and family planning cannot be separated from HIV education.
So despite the progress made in maternal and child health, the headlines are fair: HIV is the predominant health concern in Lesotho. Continued development in all sectors of Lesotho is contingent upon the 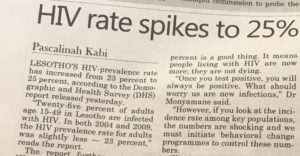 management of the HIV crisis. But if the reaction to the 2014 LDHS is any indication, stakeholders in Lesotho are poised to make data-driven decisions and to further mobilize resources to change the course of health in Lesotho.
management of the HIV crisis. But if the reaction to the 2014 LDHS is any indication, stakeholders in Lesotho are poised to make data-driven decisions and to further mobilize resources to change the course of health in Lesotho.


