DHS Data Users: Insights on Health System Quality from the Service Provision Assessments

© 2017 Magali Rochat/VectorWorks, Courtesy of Photoshare
This new blog series, DHS Data Users, captures examples of how you, the data user, have incorporated data from DHS, MIS, and/or SPA surveys into your analyses, at your institution, or to influence policies or programs. If you are interested in being featured in the ‘DHS Data Users’ blog series, let us know here by submitting your example of DHS Program data use.
The year 2018 saw an upswell of interest in health system quality with the publication of three global reports highlighting critical deficits in quality in health systems in low- and middle-income countries [1,2,3]. Much of the empirical basis for these reports was drawn from the Service Provision Assessments (SPA), the lesser-known surveys conducted by The Demographic and Health Surveys (DHS) Program, which provide comprehensive assessments of health systems in low-resource settings from Haiti to Nepal.
These surveys include a detailed audit of facility resources, provider interviews, direct observations of primary care services, and exit interviews with patients or caretakers. Each assessment is a sample of the complete health system (public and private) or in some cases a complete census. The resulting wealth of data enables assessment of structural inputs to quality of care, the care process – both competent care and user experience – and some outcomes from care, primarily user confidence in the health system. A small but increasing number of researchers is delving into all the SPA data have to offer. Among the insights the SPA surveys have yielded just from my own research are:
 Most health systems assessed are not fully prepared for basic health care.
Most health systems assessed are not fully prepared for basic health care.
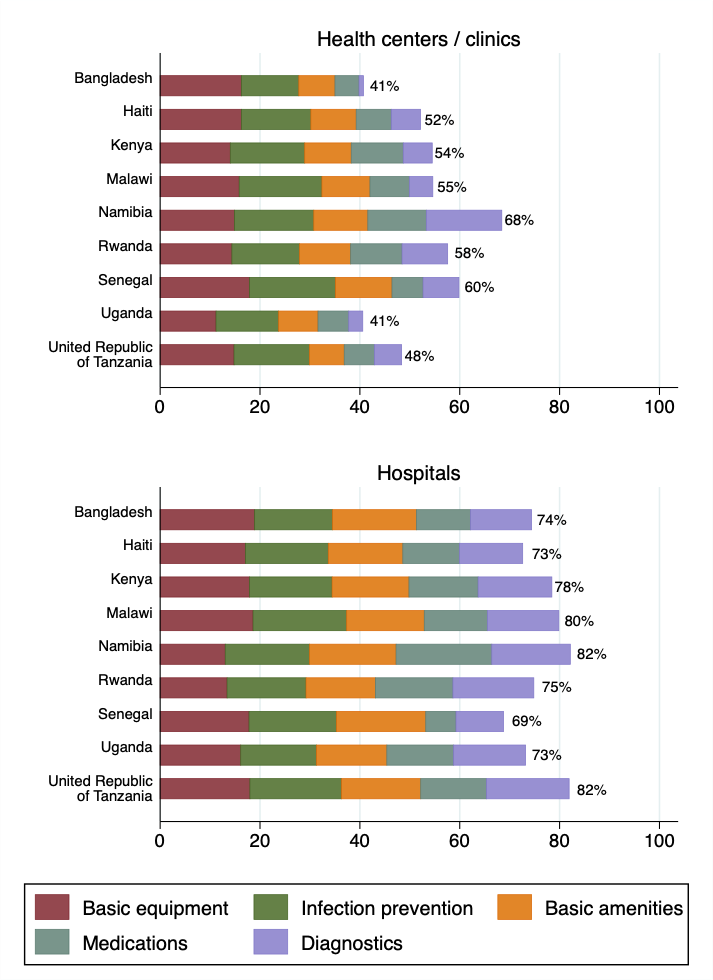
A comparative study of 8,443 facilities in 9 countries based on SPA surveys between 2007 and 2015 found that hospitals averaged between 69% (Senegal 2012-2014) and 82% (Tanzania 2015, Namibia 2009) on the service readiness index defined by the World Health Organization for primary health facilities. Non-hospitals achieved at best 68% readiness (Namibia 2009) and at worst only 41% (Uganda 2007, Bangladesh 2014) [4]. Within primary care services – antenatal care, family planning, and sick child care – service-specific service readiness is not highly predictive of competent care being delivered.- Across facilities with a similar level of readiness, provider adherence to clinical guidelines varied widely. Correlation between readiness and observed clinical quality was more consistent for observations of labor and delivery, though only two SPA surveys include these data [5].
- In Kenya
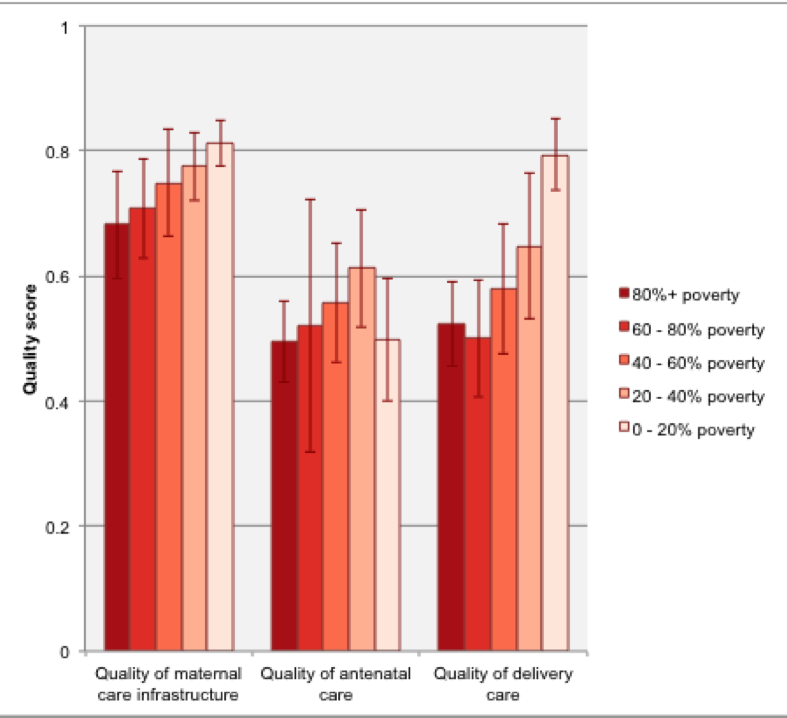 , where the 2010 SPA did include direct observation of labor and delivery, both structural quality of maternity care and observed clinical quality was higher in facilities in wealthier areas than facilities in poorer areas, with women in the poorest areas receiving care that complied with only half of recommended clinical guidelines on average [6].
, where the 2010 SPA did include direct observation of labor and delivery, both structural quality of maternity care and observed clinical quality was higher in facilities in wealthier areas than facilities in poorer areas, with women in the poorest areas receiving care that complied with only half of recommended clinical guidelines on average [6]. - Across 8 countries, adherence to clinical guidelines was lower in sick child care, where providers completed only 38% of the standard Integrated Management of Childhood Illness (IMCI) items, than in family planning (46%) and antenatal care (57%) [7]. The median sick child consultation lasted only 8 minutes [8]. Focusing specifically on Malawi, where the survey team conducted a limited re-examination of sick children, providers diagnosed pneumonia in only 1 in 5 children who showed symptoms of pneumonia per the IMCI guidelines [9].
- Analysis of the 2013-2014 Malawi SPA survey with a simultaneous household survey suggested that poor quality care may contribute to avertable neonatal mortality, with a predicted prevalence of neonatal mortality of 28.3 deaths per 1,000 in lower quality facilities and 5.2 deaths per 1,000 in higher quality facilities, among women who would choose higher quality if it were more accessible to them [10].
As attention shifts from describing health system quality to improving it at scale, robust and ongoing measurement will be an essential tool for governments and researchers alike, particularly the direct observation of care delivery and perspective from patients themselves that makes the SPA such a unique and valuable resource.
Written by Dr. Hannah Leslie

Dr. Hannah Leslie is a Research Associate at the Harvard Chan School of Public Health; she served as the Measurement Research Lead for the Lancet Global Health Commission on High-Quality Health Systems in the SDG Era. She received her MPH and Ph.D. in Epidemiology from the University of California, Berkeley. Her research has made extensive use of the Service Provision Assessment surveys to 1) develop metrics of structure and process quality in LMICs, 2) describe current quality of care, and 3) assess predictors and effects of poor quality. Her recent work focuses on effective coverage calculations, patient experience measurement, and quality of care as a driver of HIV testing and treatment retention.


The quality of the health systems needs improvement very much. There are a lot of cities, villages where proper health facilities are not available and if they are provided, not everyone can reach them. Thanks for updating people about this issue. It would be nice if you share some more information on this.
Pediatric Dentist Mandarin Florida